This is “Nutrition through the Life Cycle: From Pregnancy to the Toddler Years”, chapter 12 from the book An Introduction to Nutrition (v. 1.0). For details on it (including licensing), click here.
For more information on the source of this book, or why it is available for free, please see the project's home page. You can browse or download additional books there. To download a .zip file containing this book to use offline, simply click here.
Chapter 12 Nutrition through the Life Cycle: From Pregnancy to the Toddler Years
Big Idea
Breastfeeding promotion and support greatly influences infant health.

The choice to breastfeed is one that all new mothers face. Support from family members, friends, employers, and others can greatly help with both the decision-making process during pregnancy and the practice of breastfeeding after the baby’s birth.
© Thinkstock
The World Health Organization (WHO) recommends that infants should be given only breast milk for the first six months of life. Exclusive breastfeeding is one of the best ways a mother can support the growth and protect the health of her infant child. Breast milk contains all of the nutrients that a newborn requires and gives a child the best start to a healthy life. Many women want to breastfeed their babies. Unfortunately, a mother’s intention alone may not be enough to make this practice possible. Around the world, less than 40 percent of infants under the age of six months are breastfed exclusively.World Health Organization. “10 Facts on Breastfeeding.” Accessed February 21, 2012. http://www.who.int/features/factfiles/breastfeeding/en/. In the United States, about 75 percent of babies start out being breastfed. Yet by the age of six months, when solid foods should begin to be introduced into a child’s diet along with breast milk, only 15 percent of infants in the United States were still breastfed exclusively, according to the Centers for Disease Control and Prevention (CDC).Centers for Disease Control and Prevention. “Breastfeeding: Promotion and Support.” Last updated August 2, 2011. http://www.cdc.gov/breastfeeding/promotion/index.htm. However, the approval and assistance of family members, friends, employers, health-care providers, and policymakers can make an enormous difference and provide the needed promotion and support for mothers who wish to breastfeed their children.
Education about breastfeeding typically begins with health-care providers. During prenatal care and often soon after a woman has given birth, doctors, nurses, and other clinicians can explain the benefits of breastfeeding and describe the proper technique. Nearly all births in the United States and Canada occur in hospital settings, and hospital practices in labor, delivery, postpartum care, and discharge planning can inform and support women who want to breastfeed. Once a new mother has left the hospital for home, she needs access to a trained individual who can provide consistent information. International Board Certified Lactation Consultants (IBCLCs) are health-care professionals (often a registered nurse or registered dietitian) certified in breastfeeding management that work with new mothers to solve problems and educate families about the benefits of this practice. Research shows that breastfeeding rates are higher among women who had infants in hospitals that make IBCLCs available to new mothers, rather than those who gave birth in institutions without these professionals on staff.US Department of Health and Human Services, Office of the Surgeon General. “Executive Summary: The Surgeon General’s Call to Action to Support Breastfeeding.” January 20, 2011. http://www.surgeongeneral.gov/topics/breastfeeding/executivesummary.pdf. In addition, spouses, partners, and other family members can play critical roles in helping a pregnant woman make the decision to breastfeed and assisting with feeding after the baby is born.
Employment can also factor into a woman’s decision to breastfeed or her ability to maintain the practice. Employed mothers have been less likely to initiate breastfeeding and tend to breastfeed for a shorter period of time than new mothers who are not employed or who have lengthy maternity leaves. In 2010 in the United States, the passage of the Affordable Care Act (ACA) called for employers to provide accommodations within the workplace for new mothers to pump breast milk. This law requires a private and clean space within the workplace, other than a restroom, along with adequate break time for a woman to express milk.US Department of Health and Human Services, Office of the Surgeon General. “Executive Summary: The Surgeon General’s Call to Action to Support Breastfeeding.” January 20, 2011. http://www.surgeongeneral.gov/topics/breastfeeding/executivesummary.pdf.
Members of a community can also promote and support breastfeeding. New mothers can join peer counseling groups or turn to other women within their community who have previous experience with breastfeeding. In addition, community-based programs can provide education and support. The US Department of Agriculture’s Women, Infants, and Children program provides information on breastfeeding for low-income families. Launched in 2004, the Loving Support program combines peer counseling with breastfeeding promotion efforts to increase duration rates across the United States. La Leche League is an international program that provides mother-to-mother support, encouragement, and education about breastfeeding for women around the world.
You Decide
How can you help to promote and support breastfeeding practices in your community?
Although breastfeeding should be recommended and encouraged for almost all new mothers, it is important to remember that the decision to breastfeed is a personal choice and women should not be made to feel guilty if they cannot, or choose not, to breastfeed their infants. In some rare cases, a woman is unable to breastfeed or it is not in the baby’s best interest.
Nutritional choices that parents make, such as the decision to breastfeed or bottle-feed, not only affect early childhood development, but also a child’s health and wellness later in life. Therefore, it is imperative to promote and support the best practices for the well-being of infants and mothers alike. Throughout this chapter, we will examine how dietary choices—from daily caloric intake for pregnant women to serving sizes for toddlers—impact health and wellness during pregnancy and the early childhood years.
Video 12.1
Breastfeeding and Working
(click to see video)This video from the Colorado Breastfeeding Coalition focuses on the importance of making workplace accommodations for employees who are breastfeeding their infants.
12.1 The Human Life Cycle
Learning Objectives
- Identify and define the different stages of the human life cycle.
- Explain how the human body develops from infancy through the toddler years.
According to the American Journal of Clinical Nutrition, the human life span, or the maximum length of time possible for human life, is 130 years.Ordovas, J. M. “Living Well to 100: Nutrition, Genetics, Inflammation.” Am J Clin Nutr 83 (2006): 401S490S. Human bodies change significantly over time, and food is the fuel for those changes. People of all ages need the same basic nutrients—essential amino acids, carbohydrates, essential fatty acids, and twenty-eight vitamins and minerals—to sustain life and health. However, the amounts of nutrients needed differ. Throughout the human life cycleThe span of a human life, which consists of different stages, including childhood, adolescence, adulthood, and old age., the body constantly changes and goes through different periods known as stages. The major stages of the human life cycle are defined as follows:
- Pregnancy. The development of a zygote into an embryo and then into a fetus in preparation for childbirth.
- Infancy. The earliest part of childhood. It is the period from birth through age one.
- Toddler years. Occur during ages two and three and are the end of early childhood.
- Childhood. Takes place from ages four to eight.
- Puberty. The period from ages nine to thirteen, which is the beginning of adolescence.
- Older adolescence. The stage that takes place between ages fourteen and eighteen.
- Adulthood. The period from adolescence to the end of life and begins at age nineteen.
- Middle age. The period of adulthood that stretches from age thirty-one to fifty.
- Senior years, or old age. Extend from age fifty-one until the end of life.
Changes during Pregnancy
This ultrasound image shows a four-month-old fetus.
© Thinkstock
In this chapter, we will focus on the human life cycle from the prenatal period into early childhood. We begin with pregnancy, a developmental marathon that lasts about forty weeks. It begins with the first trimester (weeks one to week twelve), extends into the second trimester (weeks thirteen to week twenty-seven), and ends with the third trimester (week twenty-eight to birth). At conception, a sperm cell fertilizes an egg cell, creating a zygote. The zygote rapidly divides into multiple cells to become an embryo and implants itself in the uterine wall, where it develops into a fetus. Some of the major changes that occur include the branching of nerve cells to form primitive neural pathways at eight weeks. At the twenty-week mark, physicians typically perform an ultrasound to acquire information about the fetus and check for abnormalities. By this time, it is possible to know the sex of the baby. At twenty-eight weeks, the unborn baby begins to add body fat in preparation for life outside of the womb.Elaine U. Polan, RNC, MS and Daphne R. Taylor, RN, MS, Journey Across the Life Span: Human Development and Health Promotion (Philadelphia: F.A. Davis Company, 2003), 81–82. Throughout this entire process, a pregnant woman’s nutritional choices affect not only fetal development, but also her own health and the future health of her newborn.
Changes during Infancy
A number of major physiological changes occur during infancy. The trunk of the body grows faster than the arms and legs, while the head becomes less prominent in comparison to the limbs. Organs and organ systems grow at a rapid rate. Also during this period, countless new synapses form to link brain neurons. Two soft spots on the baby’s skull, known as fontanels, allow the skull to accommodate rapid brain growth. The posterior fontanel closes first, by the age of eight weeks. The anterior fontanel closes about a year later, at eighteen months on average. Developmental milestones include sitting up without support, learning to walk, teething, and vocalizing among many, many others. All of these changes require adequate nutrition to ensure development at the appropriate rate.Beverly McMillan, Illustrated Atlas of the Human Body (Sydney, Australia: Weldon Owen, 2008), 248.
Changes during the Toddler Years
Major physiological changes continue into the toddler years. Unlike in infancy, the limbs grow much faster than the trunk, which gives the body a more proportionate appearance. By the end of the third year, a toddler is taller and more slender than an infant, with a more erect posture. As the child grows, bone density increases and bone tissue gradually replaces cartilage. This process known as ossification is not completed until puberty.Elaine U. Polan, RNC, MS and Daphne R. Taylor, RN, MS, Journey Across the Life Span: Human Development and Health Promotion (Philadelphia: F.A. Davis Company, 2003), 108. Developmental milestones include running, drawing, toilet training, and self-feeding. How a toddler acts, speaks, learns, and eats offers important clues about their development.
Nutrition and Early Development
In this chapter and the next, we will explore how the dietary decisions we make affect our health and wellness throughout the life cycle. We begin by examining the developmental changes that occur during pregnancy, infancy, and the toddler years, and how nutritional choices affect those changes. From pregnancy through the toddler years, children are entirely dependent on parents or caregivers for nutrients. Parents also help to establish a child’s eating habits and attitudes toward food. So, adults must be mindful of the choices they make and how those choices influence a young child’s development, health, and overall well-being.
Key Takeaways
- The human body constantly develops and changes throughout the human life cycle, and food provides the fuel for those changes.
- The major stages of the human life cycle include pregnancy, infancy, the toddler years, childhood, puberty, older adolescence, adulthood, middle age, and the senior years.
- Proper nutrition and exercise ensure health and wellness at each stage of the human life cycle.
Discussion Starter
- In preparation for this chapter and the next, predict how you think nutrient needs might differ at the beginning of life compared to the end of life. Then, after reading this chapter and the one that follows, discuss if your predictions were correct or incorrect.
12.2 Pregnancy and Nutrition
Learning Objectives
- Summarize prenatal nutritional requirements and dietary recommendations.
- Discuss the most important nutritional concerns during pregnancy.
- Explore the relationship between fetal development and nutritional choices.
It is crucial to consume healthy foods at every phase of life, beginning in the womb. Good nutrition is vital for any pregnancy and not only helps an expectant mother remain healthy, but also impacts the development of the fetus and ensures that the baby thrives in infancy and beyond. During pregnancy, a woman’s needs increase for certain nutrients more than for others. If these nutritional needs are not met, infants could suffer from low birth weight (a birth weight less than 5.5 pounds, which is 2,500 grams), among other developmental problems. Therefore, it is crucial to make careful dietary choices.
The Early Days of Pregnancy
For medical purposes, pregnancy is measured from the first day of a woman’s last menstrual period until childbirth, and typically lasts about forty weeks. Major changes begin to occur in the earliest days, often weeks before a woman even knows that she is pregnant. During this period, adequate nutrition supports cell division, tissue differentiation, and organ development. As each week passes, new milestones are reached. Therefore, women who are trying to conceive should make proper dietary choices to ensure the delivery of a healthy baby. Fathers-to-be should also consider their eating habits. A sedentary lifestyle and a diet low in fresh fruits and vegetables may affect male fertility. Men who drink too much alcohol may also damage the quantity and quality of their sperm.Mayo Clinic. “Healthy Sperm: Improving Your Fertility.” © 1998–2012 Mayo Foundation for Medical Education and Research. Accessed February 21, 2012. http://www.mayoclinic.com/health/fertility/MC00023. For both men and women, adopting healthy habits also boosts general well-being and makes it possible to meet the demands of parenting.
Tools for Change
A pregnancy may happen unexpectedly. Therefore, it is important for all women of childbearing age to get 400 micrograms of folate per day prior to pregnancy and 600 micrograms per day during pregnancy. Folate, which is also known as folic acid, is crucial for the production of DNA and RNA and the synthesis of cells. A deficiency can cause megaloblastic anemia, or the development of abnormal red blood cells, in pregnant women. It can also have a profound affect on the unborn baby. Typically, folate intake has the greatest impact during the first eight weeks of pregnancy, when the neural tube closes. The neural tube develops into the fetus’s brain, and adequate folate reduces the risk of brain abnormalities or neural tube defects, which occur in one in a thousand pregnancies in North America each year. This vital nutrient also supports the spinal cord and its protective coverings. Inadequate folic acid can result in birth defects, such as spina bifida, which is the failure of the spinal column to close. The name “folate” is derived from the Latin word folium for leaf, and leafy green vegetables such as spinach and kale are excellent sources of it. Folate is also found in legumes, liver, and oranges. Additionally, since 1998, food manufacturers have been required to add folate to cereals and other grain products.MedlinePlus, a service of the National Institutes of Health. “Folic Acid.” © 1995–2012 Therapeutic Research Faculty, publishers of Natural Medicines Comprehensive Database, Prescriber’s Letter, Pharmacist’s Letter. Last reviewed August 7, 2011. http://www.nlm.nih.gov/medlineplus/druginfo/natural/1017.html.
Weight Gain during Pregnancy
During pregnancy, a mother’s body changes in many ways. One of the most notable and significant changes is weight gain. If a pregnant woman does not gain enough weight, her unborn baby will be at risk. Poor weight gain, especially in the third trimester, could result not only in low birth weight, but also infant mortality and intellectual disabilities. Therefore, it is vital for a pregnant woman to maintain a healthy weight, and her weight prior to pregnancy has a major affect. Infant birth weight is one of the best indicators of a baby’s future health. Pregnant women of normal weight should gain between 25 and 35 pounds in total through the entire pregnancy. The precise amount that a mother should gain usually depends on her beginning body mass index (BMI). See Table 12.1 "Body Mass Index and Pregnancy" for The Institute of Medicine (IOM) recommendations.
Table 12.1 Body Mass Index and Pregnancy
| Prepregnancy BMI | Weight Category | Recommended Weight Gain |
|---|---|---|
| Below 18.5 | Underweight | 28–40 lbs. |
| 18.5–24.9 | Normal | 25–35 lbs. |
| 25.0–29.9 | Overweight | 15–25 lbs. |
| Above 30.0 | Obese (all classes) | 11–20 lbs. |
Source: Institute of Medicine. “Weight Gain during Pregnancy: Reexamining the Guidelines.” May 2009. http://www.iom.edu/~/media/Files/Report%20Files/2009/Weight-Gain-During-Pregnancy-Reexamining-the-Guidelines/Resource%20Page%20-%20Weight%20Gain%20During%20Pregnancy.pdf.
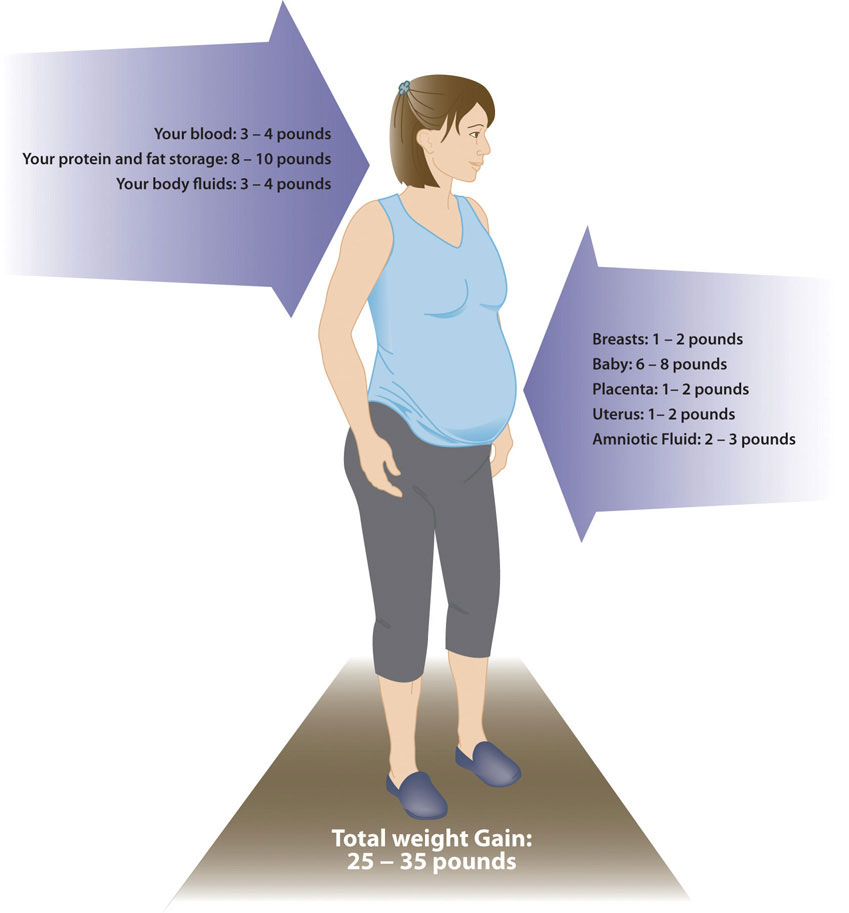
The weight an expectant mother gains during pregnancy is almost all lean tissue, including the placenta and fetus. Weight gain is not the only major change. A pregnant woman also will find that her breasts enlarge and that she has a tendency to retain water.
Source: Utah Department of Health, Baby Your Baby. “Weight Gain during Pregnancy.” © 2012 Baby Your Baby. http://www.babyyourbaby.org/pregnancy/during.
Starting weight below or above the normal range can lead to different complications. Pregnant women with a prepregnancy BMI below twenty are at a higher risk of a preterm delivery and an underweight infant. Pregnant women with a prepregnancy BMI above thirty have an increased risk of the need for a cesarean section during delivery. Therefore, it is optimal to have a BMI in the normal range prior to pregnancy.
Generally, women gain 2 to 5 pounds in the first trimester. After that, it is best not to gain more than one pound per week. Some of the new weight is due to the growth of the fetus, while some is due to changes in the mother’s body that support the pregnancy. Weight gain often breaks down in the following manner: 6 to 8 pounds of fetus, 1 to 2 pounds for the placenta (which supplies nutrients to the fetus and removes waste products), 2 to 3 pounds for the amniotic sac (which contains fluids that surround and cushion the fetus), 1 to 2 pounds in the breasts, 1 to 2 pounds in the uterus, 3 to 4 pounds of maternal blood, 3 to 4 pounds maternal fluids, and 8 to 10 pounds of extra maternal fat stores that will be needed for breastfeeding and delivery. Women who are pregnant with more than one fetus are advised to gain even more weight to ensure the health of their unborn babies.
The pace of weight gain is also important. If a woman puts on weight too slowly, her physician may recommend nutrition counseling. If she gains weight too quickly, especially in the third trimester, it may be the result of edema, or swelling due to excess fluid accumulation. Rapid weight gain may also result from increased calorie consumption or a lack of exercise.
Weight Loss after Pregnancy
During labor, new mothers lose some of the weight they gained during pregnancy with the delivery of their child. In the following weeks, they continue to shed weight as they lose accumulated fluids and their blood volume returns to normal. Some studies have hypothesized that breastfeeding also helps a new mother lose some of the extra weight, although research is ongoing.Stuebe, A. M., MD, MSc and J. W. Rich-Edwards, Sc. D. “The Reset Hypothesis: Lactation and Maternal Metabolism.” © Thieme Medical Publishers, Am J Perinatol 26, no.1 (2009): 81–88. doi: 10.1055/s-0028-1103034. New mothers who gain a healthy amount of weight and participate in regular physical activity during their pregnancies also have an easier time shedding weight postpregnancy. However, women who gain more weight than needed for a pregnancy typically retain that excess weight as body fat. If those few pounds increase a new mother’s BMI by a unit or more, that could lead to complications such as hypertension or Type 2 diabetes in future pregnancies or later in life.
Nutritional Requirements
As a mother’s body changes, so do her nutritional needs. Pregnant women must consume more calories and nutrients in the second and third trimesters than other adult women. However, the average recommended daily caloric intake can vary depending on activity level and the mother’s normal weight. Also, pregnant women should choose a high-quality, diverse diet, consume fresh foods, and prepare nutrient-rich meals. Steaming is the best way to cook vegetables. Vitamins are destroyed by overcooking, whereas uncooked vegetables and fruits have the highest vitamin content. It is also standard for pregnant women to take prenatal supplements to ensure adequate intake of the needed micronutrients.
Energy
During the first trimester, a pregnant woman has the same energy requirements as normal and should consume the same number of calories as usual—about 1,800 calories for a woman living a sedentary lifestyle, about 2,000 calories for a woman who is moderately active, and about 2,200 for a woman who is active. However, as the pregnancy progresses, a woman must increase her caloric intake. According to the IOM, she should consume an additional 340 calories per day during the second trimester, and an additional 450 calories per day during the third trimester. This is partly due to an increase in metabolism, which rises during pregnancy and contributes to increased energy needs. A woman can easily meet these increased needs by consuming more nutrient-dense foods. For example, an additional 340 calories could include a medium-sized banana (about 100 calories), a cup of nonfat yogurt with fruit on the bottom (about 140 calories), and a slice of whole-wheat toast (about 75 calories).
Carbohydrates
The recommended daily allowance, or RDA, of carbohydrates during pregnancy is about 175 to 265 grams per day to fuel fetal brain development. The best food sources for pregnant women include whole-grain breads and cereals, brown rice, root vegetables, legumes, and fruits. These and other unrefined carbohydrates provide nutrients, phytochemicals, antioxidants, and fiber. These foods also help to build the placenta and supply energy for the growth of the unborn baby. Refined carbohydrates, such as white bread, cookies and other baked desserts, pretzels, and chips are nutritionally deficient and should be kept to a minimum.
Protein
During pregnancy, extra protein is needed for the synthesis of new maternal and fetal tissues. Protein builds muscle and other tissues, enzymes, antibodies, and hormones in both the mother and the unborn baby. Additional protein also supports increased blood volume and the production of amniotic fluid. The RDA of protein during pregnancy is 71 grams per day, which is 25 grams above the normal recommendation. However, in most instances, there is no need for a pregnant woman to make an effort to increase protein intake as long as she has a normal appetite, because even nonpregnant women in North America typically eat that much protein. Protein should be derived from healthy sources, such as lean red meat, white-meat poultry, legumes, nuts, seeds, eggs, and fish. Low-fat milk and other dairy products also provide protein, along with calcium and other nutrients.
Fat
There are no specific recommendations for fats in pregnancy, apart from following normal dietary guidelines. Fats should make up 25 to 35 percent of daily calories, and those calories should come from healthy fats, such as avocados. Foods with unhealthy fats, including French fries and other fast food, should be avoided. Also, it is not recommended for pregnant women to be on a very low-fat diet, since it would be hard to meet the needs of essential fatty acids and fat-soluble vitamins. Fatty acids are important during pregnancy because they support the baby’s brain and eye development. In particular, the brain depends on omega-3 and omega-6 fatty acids, such as the kind found in salmon and sunflower or safflower oil, for function, structure, and growth. Fats can also help the placenta grow and may help to prevent premature birth and low birth weight.
Fiber

Fresh fruit and whole grains, such as a bowl of muesli, are excellent sources of fiber during a pregnancy.
© Thinkstock
Ideally, a pregnant woman should eat 25 to 30 grams of dietary fiber per day. There are two types of fiber, and pregnant women should consume both. Insoluble fiberFiber that is metabolically inert, which means it does not break down as it passes through the digestive system. Insoluble fiber absorbs water and adds bulk to stool, expediting the passage of food and waste. acts as a natural laxative, which softens stools and speeds the elimination of waste material through the colon to avoid constipation. Sources of insoluble fiber include whole grains, fruits, vegetables, dried peas, and beans. Soluble fiberFiber that attracts water and turns to gel, which slows digestion. Soluble fiber is readily fermented in the colon by bacteria into gases and waste byproducts. has little effect on the intestines, however it helps to lower blood-cholesterol levels and regulate blood glucose. Sources of soluble fiber include fruits, vegetables, and beans, along with oats, barley, and other fiber-filled whole grains.
Fluids
Fluid intake must also be monitored. According to the IOM, pregnant women should drink 2.3 liters (about 10 cups) of liquids per day to provide enough fluid for blood production. It is also important to drink liquids during physical activity or when it is hot and humid outside, to replace fluids lost to perspiration. The combination of a high-fiber diet and lots of liquids also helps to eliminate waste.US Department of Health and Human Services, Office on Women’s Health. “Pregnancy: Body Changes and Discomforts.” Last updated September 27, 2010. http://www.womenshealth.gov/pregnancy/you-are-pregnant/body-changes -discomforts.cfm.
Vitamins and Minerals
Pregnancy requires certain conditionally essential nutrientsNutrients that are supplied only under special conditions or circumstances, such as pregnancy, stress, illness, or aging., which are nutrients that are supplied only under special conditions, such as stress, illness, or aging. The daily requirements for nonpregnant women change with the onset of a pregnancy. Taking a daily prenatal supplement or multivitamin helps to meet many nutritional needs. However, most of these requirements should be fulfilled with a healthy diet. The following table compares the normal levels of required vitamins and minerals to the levels needed during pregnancy. For pregnant women, the RDA of nearly all vitamins and minerals increases.
Table 12.2 Recommended Nutrient Intakes during Pregnancy
| Nutrient | Nonpregnant Women | Pregnant Women |
|---|---|---|
| Vitamin A (mcg) | 700.0 | 770.0 |
| Vitamin B6 (mg) | 1.5 | 1.9 |
| Vitamin B12 (mcg) | 2.4 | 2.6 |
| Vitamin C (mg) | 75.0 | 85.0 |
| Vitamin D (mcg) | 5.0 | 5.0 |
| Vitamin E (mg) | 15.0 | 15.0 |
| Calcium (mg) | 1,000.0 | 1,000.0 |
| Folate (mcg) | 400.0 | 600.0 |
| Iron (mg) | 18.0 | 27.0 |
| Magnesium (mg) | 320.0 | 360.0 |
| Niacin (B3) (mg) | 14.0 | 18.0 |
| Phosphorus | 700.0 | 700.0 |
| Riboflavin (B2) (mg) | 1.1 | 1.4 |
| Thiamine (B1) (mg) | 1.1 | 1.4 |
| Zinc (mg) | 8.0 | 11.0 |
Source: Institute of Medicine. “Nutrition during Pregnancy: Part I: Weight Gain, Part II: Nutrient Supplements.” January 1, 1990. http://iom.edu/Reports/1990/Nutrition-During-Pregnancy-Part-I-Weight-Gain-Part-II-Nutrient-Supplements.aspx.
The micronutrients involved with building the skeleton—vitamin D, calcium, phosphorus, and magnesium—are crucial during pregnancy to support fetal bone development. Although the levels are the same as those for nonpregnant women, many women do not typically consume adequate amounts and should make an extra effort to meet those needs.
There is an increased need for all B vitamins during pregnancy. Adequate vitamin B6 supports the metabolism of amino acids, while more vitamin B12 is needed for the synthesis of red blood cells and DNA. Additional zinc is crucial for cell development and protein synthesis. The need for vitamin A also increases, and extra iron intake is important because of the increase in blood supply during pregnancy and to support the fetus and placenta. Iron is the one micronutrient that is almost impossible to obtain in adequate amounts from food sources only. Therefore, even if a pregnant woman consumes a healthy diet, there still is a need to take an iron supplement, in the form of ferrous salts. Also remember that folate needs increase during pregnancy to 600 micrograms per day to prevent neural tube defects. This micronutrient is crucial for fetal development because it helps produce the extra blood a woman’s body requires during pregnancy.
For most other minerals, recommended intakes are similar to those for nonpregnant women, although it is crucial for pregnant women to make sure to meet the RDAs to reduce the risk of birth defects. In addition, pregnant mothers should avoid exceeding any recommendations. Taking megadose supplements can lead to excessive amounts of certain micronutrients, such as vitamin A and zinc, which may produce toxic effects that can also result in birth defects.
Guide to Eating during Pregnancy
While pregnant women have an increased need for energy, vitamins, and minerals, energy increases are proportionally less than other macronutrient and micronutrient increases. So, nutrient-dense foods, which are higher in proportion of macronutrients and micronutrients relative to calories, are essential to a healthy diet. Examples of nutrient-dense foods include fruits, vegetables, whole grains, peas, beans, reduced-fat dairy, and lean meats. Pregnant women should be able to meet almost all of their increased needs via a healthy diet. However, expectant mothers should take a prenatal supplement to ensure an adequate intake of iron and folate. Here are some additional dietary guidelines for pregnant women:US Department of Health and Human Services, Office on Women’s Health. “Healthy Pregnancy: Do’s and Don’ts.” Last updated March 5, 2009. http://www.womenshealth.gov/publications/our-publications/pregnancy-dos -donts.pdf.
- Eat iron-rich or iron-fortified foods, including meat or meat alternatives, breads, and cereals, to help satisfy increased need for iron and prevent anemia.
- Include vitamin C-rich foods, such as orange juice, broccoli, or strawberries, to enhance iron absorption.
- Eat a well-balanced diet, including fruits, vegetables, whole grains, calcium-rich foods, lean meats, and a variety of cooked seafood (excluding fish that are high in mercury, such as swordfish and shark).
- Drink additional fluids, water especially.
Foods to Avoid
A number of substances can harm a growing fetus. Therefore, it is vital for women to avoid them throughout a pregnancy. Some are so detrimental that a woman should avoid them even if she suspects that she might be pregnant. For example, consumption of alcoholic beverages results in a range of abnormalities that fall under the umbrella of fetal alcohol spectrum disorders. They include learning and attention deficits, heart defects, and abnormal facial features. Alcohol enters the unborn baby via the umbilical cord and can slow fetal growth, damage the brain, or even result in miscarriage. The effects of alcohol are most severe in the first trimester, when the organs are developing. As a result, there is no safe amount of alcohol that a pregnant woman can consume. Although pregnant women in the past may have participated in behavior that was not known to be risky at the time, such as drinking alcohol or smoking cigarettes, today we know that it is best to avoid those substances completely to protect the health of the unborn baby.
Pregnant women should also limit caffeine intake, which is found not only in coffee, but also tea, colas, cocoa, chocolate, and some over-the-counter painkillers. Some studies suggest that very high amounts of caffeine have been linked to babies born with low birth weights. The American Journal of Obstetrics and Gynecology released a report, which found that women who consume 200 milligrams or more of caffeine a day (which is the amount in 10 ounces of coffee or 25 ounces of tea) increase the risk of miscarriage.Weng X, Odouli R, and Li D-K. “Maternal caffeine consumption during pregnancy and the risk of miscarriage: a prospective cohort study.” Am J Obstet Gynecol 2008;198:279.e1-279.e8. Consuming large quantities of caffeine affects the pregnant mother as well, leading to irritability, anxiety, and insomnia. Most experts agree that small amounts of caffeine each day are safe (about one 8-ounce cup of coffee a day or less).American Medical Association, Complete Guide to Prevention and Wellness (Hoboken, NJ: John Wiley & Sons, Inc., 2008), 495. However, that amount should not be exceeded.
Foodborne Illness
For both mother and child, foodborne illness can cause major health problems. For example, the foodborne illness caused by the bacteria Listeria monocytogenes can cause spontaneous abortion and fetal or newborn meningitis. According to the CDC, pregnant women are twenty times more likely to become infected with this disease, which is known as listeriosis, than nonpregnant, healthy adults. Symptoms include headaches, muscle aches, nausea, vomiting, and fever. If the infection spreads to the nervous system, it can result in a stiff neck, convulsions, or a feeling of disorientation.American Pregnancy Association. “Listeria and Pregnancy.” © 2000–2012 American Pregnancy Association. http://www.americanpregnancy.org/pregnancycomplications/listeria.html.
Foods more likely to contain the bacteria are unpasteurized dairy products, especially soft cheeses, and also smoked seafood, hot dogs, paté, cold cuts, and uncooked meats. To avoid consuming contaminated foods, women who are pregnant or breastfeeding should take the following measures:
- Thoroughly rinse fruits and vegetables before eating them
- Keep cooked and ready-to-eat food separate from raw meat, poultry, and seafood
- Store food at 40° F (4° C) or below in the refrigerator and at 0° F (−18° C) in the freezer
- Refrigerate perishables, prepared food, or leftovers within two hours of preparation or eating
- Clean the refrigerator regularly and wipe up any spills right away
- Check the expiration dates of stored food once per week
You will learn more about foodborne illness and its consequences in Chapter 14 "Nutrition and Society: Food Politics and Perspectives" and Chapter 15 "Achieving Optimal Health: Wellness and Nutrition".
Food Contaminants
It is always important to avoid consuming contaminated food to prevent food poisoning. This is especially true during pregnancy. Heavy metal contaminants, particularly mercury, lead, and cadmium, pose risks to pregnant mothers. As a result, vegetables should be washed thoroughly or have their skins removed to avoid heavy metals.
Pregnant women can eat fish, ideally 8 to 12 ounces of different types each week. Expectant mothers are able to eat cooked shellfish such as shrimp, farm-raised fish such as salmon, and a maximum of 6 ounces of albacore, or white, tuna. However, they should avoid fish with high methyl mercury levels, such as shark, swordfish, tilefish, and king mackerel. Pregnant women should also avoid consuming raw shellfish to avoid foodborne illness. The Environmental Defense Fund eco-rates fish to provide guidelines to consumers about the safest and most environmentally friendly choices. You can find ratings for fish and seafood at http://www.edf.org.
Physical Activity during Pregnancy

Walking is an excellent way for an expectant mother to get moderate exercise.
© Thinkstock
For most pregnant women, physical activity is a must and is recommended in the 2010 Dietary Guidelines for Americans. Regular exercise of moderate intensity, about thirty minutes per day most days of the week, keeps the heart and lungs healthy. It also helps to improve sleep and boosts mood and energy levels. In addition, women who exercise during pregnancy report fewer discomforts and may have an easier time losing excess weight after childbirth. Brisk walking, swimming, or an aerobics class geared toward expectant mothers are all great ways to get exercise during a pregnancy. Healthy women who already participate in vigorous activities, such as running, can continue doing so during pregnancy provided they discuss an exercise plan with their physicians.
However, pregnant women should avoid pastimes that could cause injury, such as soccer, football, and other contact sports, or activities that could lead to falls, such as horseback riding and downhill skiing. It may be best for pregnant women not to participate in certain sports, such as tennis, that require you to jump or change direction quickly. Scuba diving should also be avoided because it might result in the fetus developing decompression sickness. This potentially fatal condition results from a rapid decrease in pressure when a diver ascends too quickly.National Institutes of Health, and Friends of the National Library of Medicine. “Should I Exercise During My Pregnancy?” NIH Medline Plus 3, no. 1 (Winter 2008): 26. http://www.nlm.nih.gov/medlineplus/magazine/issues/winter08/articles/winter08pg26.html.
Common Discomforts during Pregnancy
Pregnancy can lead to certain discomforts, from back strain to swollen ankles. Also, a pregnant woman is likely to experience constipation because increased hormone levels can slow digestion and relax muscles in the bowels. Constipation and pressure from growth of the uterus can result in hemorrhoids, which are another common discomfort.US Department of Health and Human Services, Office on Women’s Health. “Pregnancy: Body Changes and Discomforts.” Last updated September 27, 2010. http://www.womenshealth.gov/pregnancy/you-are-pregnant/body-changes -discomforts.cfm. Getting mild to moderate exercise and drinking enough fluids can help prevent both conditions. Also, eating a high-fiber diet softens the stools and reduces the pressure on hemorrhoids.
Heartburn can occur during the early months of pregnancy due to an increase in the hormone progesterone, and during the later months due to the expanding size of the fetus, which limits stomach contraction. Avoiding chocolate, mint, and greasy foods, and remaining upright for an hour after meals can help pregnant women avoid heartburn. In addition, it can be helpful to drink fluids between meals, instead of with food.
Other common complaints can include leg cramps and bloating. Regular exercise can help to alleviate these discomforts. A majority of pregnant women develop gastrointestinal issues, such as nausea and vomiting. Many also experience food cravings and aversions. All of these can impact a pregnant woman’s nutritional intake and it is important to protect against adverse effects.
Nausea and Vomiting
Nausea and vomiting are gastrointestinal issues that strike many pregnant women, typically in the first trimester. Nausea tends to occur more frequently than vomiting. These conditions are often referred to as “morning sickness,” although that’s something of a misnomer because nausea and vomiting can occur all day long, although it is often the worst in the first part of the day.
Increased levels of the pregnancy hormone human chorionic gonadotropin may cause nausea and vomiting, although that is speculative. Another major suspect is estrogen because levels of this hormone also rise and remain high during pregnancy. Given that a common side effect of estrogen-containing oral contraceptives is nausea this hormone likely has a role. Nausea usually subsides after sixteen weeks, possibly because the body becomes adjusted to higher estrogen levels.
It can be useful for pregnant women to keep a food diary to discover which foods trigger nausea, so they can avoid them in the future. Other tips to help avoid or treat nausea and vomiting include the following:
- Avoid spicy foods
- Avoid strong or unusual odors
- Eat dry cereal, toast, or crackers
- Eat frequent, small meals
- Consume more unrefined carbohydrates
- Get moderate aerobic exercise
- Drink ginger tea, which aids in stomach upset
- Seek fresh air when a bout of nausea comes on
A severe form of nausea and vomiting is a condition known as hyperemesis gravidarum. It is marked by prolonged vomiting, which can result in dehydration and require hospitalization. This disorder is relatively rare and impacts only 0.3 to 2 percent of all pregnant women.Eliakim, R., O. Abulafia, and D. M. Sherer. “Hyperemesis Gravidarum: A Current Review.” Am J Perinatol 17, no. 4 (2000): 207–18.
Food Cravings and Aversions
Food aversions and cravings do not have a major impact unless food choices are extremely limited. The most common food aversions are milk, meats, pork, and liver. For most women, it is not harmful to indulge in the occasional craving, such as the desire for pickles and ice cream. However, a medical disorder known as pica is willingly consuming foods with little or no nutritive value, such as dirt, clay, and laundry starch. In some places this is a culturally accepted practice. However, it can be harmful if these substances take the place of nutritious foods or contain toxins.
Complications during Pregnancy
Expectant mothers may face different complications during the course of their pregnancy. They include certain medical conditions that could greatly impact a pregnancy if left untreated, such as gestational hypertension and gestational diabetes, which have diet and nutrition implications.
Gestational Hypertension
Gestational hypertensionA possible complication of pregnancy characterized by raised blood pressure levels. is a condition of high blood pressure during the second half of pregnancy. Also referred to as pregnancy-induced hypertension, this condition affects about 6 to 8 percent of all pregnant women. First-time mothers are at a greater risk, along with women who have mothers or sisters who had gestational hypertension, women carrying multiple fetuses, women with a prior history of high blood pressure or kidney disease, and women who are overweight or obese when they become pregnant.
Hypertension can prevent the placenta from getting enough blood, which would result in the baby getting less oxygen and nutrients. This can result in low birth weight, although most women with gestational hypertension can still deliver a healthy baby if the condition is detected and treated early. Some risk factors can be controlled, such as diet, while others cannot, such as family history. If left untreated, gestational hypertension can lead to a serious complication called preeclampsiaA possible complication of pregnancy marked by elevated blood pressure and high levels of protein in the urine., which is sometimes referred to as toxemia. This disorder is marked by elevated blood pressure and protein in the urine and is associated with swelling. To prevent preeclampsia, the WHO recommends increasing calcium intake for women consuming diets low in that micronutrient, administering a low dosage of aspirin (75 milligrams), and increasing prenatal checkups.World Health Organization. “WHO Recommendations for Prevention and Treatment of Pre-eclampsia and Eclampsia.” 2011. Accessed June 8, 2012. http://whqlibdoc.who.int/publications/2011/9789241548335_eng.pdf.
Video 12.2
Gestational Hypertension and Preeclampsia
(click to see video)This video focuses on the signs and risk factors of gestational hypertension and preeclampsia.
Gestational Diabetes
About 4 percent of pregnant women suffer from a condition known as gestational diabetesA possible complication of pregnancy characterized by elevated blood glucose levels., which is abnormal glucose tolerance during pregnancy. The body becomes resistant to the hormone insulin, which enables cells to transport glucose from the blood. Gestational diabetes is usually diagnosed around twenty-four to twenty-six weeks, although it is possible for the condition to develop later into a pregnancy. Signs and symptoms of this disease include extreme hunger, thirst, or fatigue. If blood sugar levels are not properly monitored and treated, the baby might gain too much weight and require a cesarean delivery. Diet and regular physical activity can help to manage this condition. Most patients who suffer from gestational diabetes also require daily insulin injections to boost the absorption of glucose from the bloodsteam and promote the storage of glucose in the form of glycogen in liver and muscle cells. Gestational diabetes usually resolves after childbirth, although some women who suffer from this condition develop Type 2 diabetes later in life, particularly if they are overweight.
Key Takeaways
- During pregnancy, it is imperative that a woman meet the nutritional needs both she and her unborn child require, which includes an increase in certain micronutrients, such as iron and folate.
- Starting BMI determines how much weight a woman needs to gain throughout her pregnancy. In an average pregnancy, a woman gains an extra 30 pounds.
- During the second and third trimesters, a woman’s energy requirements increase by 340 calories per day for the second trimester and 450 calories per day for the third trimester.
- Common discomforts that can impact nutritional intake during pregnancy include nausea and vomiting, heartburn, and constipation.
- Gestational hypertension is a condition that impacts about 6 to 8 percent of pregnant women and results in a rise of blood pressure levels. This condition can lead to preeclampsia during a pregnancy.
- Gestational diabetes is a condition that impacts about 4 percent of pregnant women and results in a rise of blood glucose levels. This condition can lead to Type 2 diabetes later in life.
Discussion Starter
- Discuss the changing nutritional requirements for iron and vitamin A during pregnancy. Use what you know about each kind of micronutrient and its impact on the body to explain why the increase in RDA might be exponentially greater for one of these nutrients than for the other.
12.3 Infancy and Nutrition
Learning Objectives
- Summarize nutritional requirements and dietary recommendations for infants.
- Describe the physiologic basis for lactation and the specific components of breast milk.
- Discuss the benefits and barriers related to breastfeeding.
- Examine feeding problems that parents and caregivers may face with their infants.
Diet and nutrition have a major impact on a child’s development from infancy into the adolescent years. A healthy diet not only affects growth, but also immunity, intellectual capabilities, and emotional well-being. One of the most important jobs of parenting is making sure that children receive an adequate amount of needed nutrients to provide a strong foundation for the rest of their lives.
Infancy (Birth to Age One)
The term infant is derived from the Latin word infans, which means “unable to speak.” Healthy infants grow steadily, but not always at an even pace. For example, during the first year of life, height increases by 50 percent, while weight triples. Physicians and other health professionals can use growth charts to track a baby’s development process. Because infants cannot stand, length is used instead of height to determine the rate of a child’s growth. Other important developmental measurements include head circumference and weight. All of these must be tracked and compared against standard measurements for an infant’s age. Nationally-accepted growth charts are based on data collected by the National Center for Health Statistics. These charts allow for tracking trends over time and comparing with other infants among percentiles within the United States. Growth charts may provide warnings that a child has a medical problem or is malnourished. Insufficient weight or height gain during infancy may indicate a condition known as failure-to-thrive (FTT)A condition that is characterized by inadequate growth or weight gain due to any cause., which is characterized by poor growth. FTT can happen at any age, but in infancy, it typically occurs after six months. Some causes include poverty, lack of enough food, feeding inappropriate foods, and excessive intake of fruit juice.
Nutritional Requirements
Requirements for macronutrients and micronutrients on a per-kilogram basis are higher during infancy than at any other stage in the human life cycle. These needs are affected by the rapid cell division that occurs during growth, which requires energy and protein, along with the nutrients that are involved in DNA synthesis. During this period, children are entirely dependent on their parents or other caregivers to meet these needs. For almost all infants six months or younger, breast milk is the best source to fulfill nutritional requirements. An infant may require feedings eight to twelve times a day or more in the beginning. After six months, infants can gradually begin to consume solid foods to help meet nutrient needs.
Energy
Energy needs relative to size are much greater in an infant than an adult. A baby’s resting metabolic rate is two times that of an adult. The RDA to meet energy needs changes as an infant matures and puts on more weight. The IOM uses a set of equations to calculate the total energy expenditure and resulting energy needs. For example, the equation for the first three months of life is (89 x weight [kg] −100) + 175 kcal.
Based on these equations, the estimated energy requirement for infants from zero to six months of age is 472 to 645 kilocalories per day for boys and 438 to 593 kilocalories per day for girls. For infants ages six to twelve months, the estimated requirement is 645 to 844 kilocalories per day for boys and 593 to 768 kilocalories per day for girls. From the age one to age two, the estimated requirement rises to 844–1,050 kilocalories per day for boys and 768–997 kilocalories per day for girls.Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids, Institute of Medicine of the National Academies (Washington, D.C.: The National Academies Press, 2005), 169–70. How often an infant wants to eat will also change over time due to growth spurts, which typically occur at about two weeks and six weeks of age, and again at about three months and six months of age.
Macronutrients
The dietary recommendations for infants are based on the nutritional content of human breast milk. Carbohydrates make up about 45 to 65 percent of the caloric content in breast milk, which amounts to a RDA of about 130 grams. Almost all of the carbohydrate in human milk is lactose, which infants digest and tolerate well. In fact, lactose intolerance is practically nonexistent in infants. Protein makes up about 5 to 20 percent of the caloric content of breast milk, which amounts to 13 grams per day. Infants have a high need for protein to support growth and development, though excess protein (which is only a concern with bottle-feeding) can cause dehydration, diarrhea, fever, and acidosis in premature infants. About 30 to 40 percent of the caloric content in breast milk is made up of fat. A high-fat diet is necessary to encourage the development of neural pathways in the brain and other parts of the body. However, saturated fats and trans fatty acids inhibit this growth. Infants who are over the age of six months, which means they are no longer exclusively breastfed, should not consume foods that are high in these types of fats.
Micronutrients
Almost all of the nutrients that infants require can be met if they consume an adequate amount of breast milk. There are a few exceptions, though. Human milk is low in vitamin D, which is needed for calcium absorption and building bone, among other things. Therefore, breastfed children often need to take a vitamin D supplement in the form of drops. Infants at the highest risk for vitamin D deficiency are those with darker skin and no exposure to sunlight. Breast milk is also low in vitamin K, which is required for blood clotting, and deficits could lead to bleeding or hemorrhagic disease. Babies are born with limited vitamin K, so supplementation may be needed initially and some states require a vitamin K injection after birth. Also, breast milk is not high in iron, but the iron in breast milk is well absorbed by infants. After four to six months, however, an infant needs an additional source of iron other than breast milk.
Fluids
Infants have a high need for fluids, 1.5 milliliters per kilocalorie consumed compared to 1.0 milliliters per kilocalorie consumed for adults. This is because children have larger body surface area per unit of body weight and a reduced capacity for perspiration. Therefore, they are at greater risk of dehydration. However, parents or other caregivers can meet an infant’s fluid needs with breast milk or formula. As solids are introduced, parents must make sure that young children continue to drink fluids throughout the day.
Breastfeeding
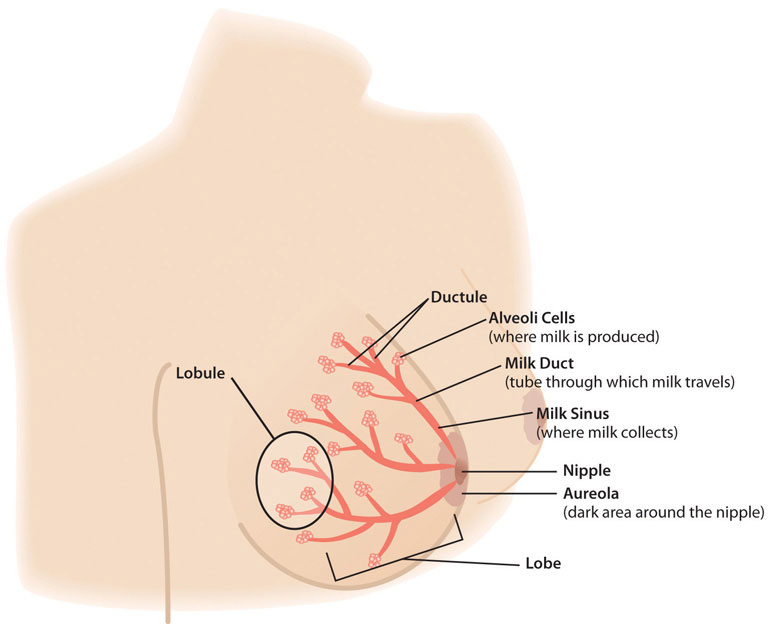
The alveoli cells produce milk. To secrete it, they contract and push milk into the ductules and the milk sinus, which collects the milk. When a nursing infant’s gums press on the areola and nipple, the sinuses squeeze the milk into the baby’s mouth. The nipple tissue becomes firmer with stimulation, which makes it more flexible and easier for the baby to grasp in the mouth.
After the birth of the baby, nutritional needs must be met to ensure that an infant not only survives, but thrives from infancy into childhood. Breastfeeding provides the fuel a newborn needs for rapid growth and development. As a result, the WHO recommends that breastfeeding be done exclusively for the first six months of an infant’s life. New mothers must also pay careful consideration to their own nutritional requirements to help their bodies recover in the wake of the pregnancy. This is particularly true for women who breastfeed their babies, which calls for an increased need in certain nutrients.
Lactation
LactationThe medical term for the process of producing and secreting breast milk. is the process that makes breastfeeding possible, and is the synthesis and secretion of breast milk. Early in a woman’s pregnancy, her mammary glands begin to prepare for milk production. Hormones play a major role in this, particularly during the second and third trimesters. At that point, levels of the hormone prolactin increase to stimulate the growth of the milk duct system, which initiates and maintains milk production. Levels of the hormone oxytocin also rise to promote the release of breast milk when the infant suckles, which is known as the milk ejection reflex. However, levels of the hormone progesterone need to decrease for successful milk production, because progesterone inhibits milk secretion. Shortly after birth, the expulsion of the placenta triggers progesterone levels to fall, which activates lactation.King, J. “Contraception and Lactation: Physiology of Lactation.” Journal of Midwifery and Women’s Health 52, no. 6 (2007): 614–20. © 2007 Elsevier Science, Inc.
New mothers need to adjust their caloric and fluid intake to make breastfeeding possible. The RDA is 330 additional calories during the first six months of lactation and 400 additional calories during the second six months of lactation. The energy needed to support breastfeeding comes from both increased intake and from stored fat. For example, during the first six months after her baby is born, the daily caloric cost for a lactating mother is 500 calories, with 330 calories derived from increased intake and 170 calories derived from maternal fat stores. This helps explain why breastfeeding may promote weight loss in new mothers. Lactating women should also drink 3.1 liters of liquids per day (about 13 cups) to maintain milk production, according to the IOM. As is the case during pregnancy, the RDA of nearly all vitamins and minerals increases for women who are breastfeeding their babies. The following table compares the recommended vitamins and minerals for lactating women to the levels for nonpregnant and pregnant women from Table 12.2 "Recommended Nutrient Intakes during Pregnancy".
Table 12.3 Recommended Nutrient Intakes during Lactation
| Nutrient | Nonpregnant Women | Pregnant Women | Lactating Women |
|---|---|---|---|
| Vitamin A (mcg) | 700.0 | 770.0 | 1,300.0 |
| Vitamin B6 (mg) | 1.5 | 1.9 | 2.0 |
| Vitamin B12 (mcg) | 2.4 | 2.6 | 2.8 |
| Vitamin C (mg) | 75.0 | 85.0 | 120.0 |
| Vitamin D (mcg) | 5.0 | 5.0 | 5.0 |
| Vitamin E (mg) | 15.0 | 15.0 | 19.0 |
| Calcium (mg) | 1,000.0 | 1,000.0 | 1,000.0 |
| Folate (mcg) | 400.0 | 600.0 | 500.0 |
| Iron (mg) | 18.0 | 27.0 | 9.0 |
| Magnesium (mg) | 320.0 | 360.0 | 310.0 |
| Niacin (B3) (mg) | 14.0 | 18.0 | 17.0 |
| Phosphorus | 700.0 | 700.0 | 700.0 |
| Riboflavin (B2) (mg) | 1.1 | 1.4 | 1.6 |
| Thiamine (B1) (mg) | 1.1 | 1.4 | 1.4 |
| Zinc (mg) | 8.0 | 11.0 | 12.0 |
Source: Institute of Medicine, http://www.iom.edu.
Calcium requirements do not change during breastfeeding because of more efficient absorption, which is the case during pregnancy, too. However, the reasons for this differ. During pregnancy, there is enhanced absorption within the gastrointestinal tract. During lactation, there is enhanced retention by the kidneys. The RDA for phosphorus, fluoride, and molybdenum also remains the same.
Components of Breast Milk
Human breast milk not only provides adequate nutrition for infants, it also helps to protect newborns from disease. In addition, breast milk is rich in cholesterol, which is needed for brain development. It is helpful to know the different types and components of breast milk, along with the nutrients they provide to enable an infant survive and thrive.
Colostrum
ColostrumA yellow fluid produced in a mother’s breasts during the first few days after delivery, prior to milk production. is produced immediately after birth, prior to the start of milk production, and lasts for several days after the arrival of the baby. Colostrum is thicker than breast milk, and is yellowish or creamy in color. This protein-rich liquid fulfills an infant’s nutrient needs during those early days. Although low in volume, colostrum is packed with concentrated nutrition for newborns. This special milk is high in fat-soluble vitamins, minerals, and immunoglobulinsProteins produced by plasma cells that function as antibodies. In infancy, immunoglobulins pass from mother to infant via breast milk and provide passive immunity for the baby. (antibodies) that pass from the mother to the baby. Immunoglobulins provide passive immunity for the newborn and protect the baby from bacterial and viral diseases.American Pregnancy Association. “Breastfeeding: Overview.” Last updated January 2012. http://www.americanpregnancy.org/firstyearoflife/breastfeedingoverview.htm.
Transitional Milk
Two to four days after birth, colostrum is replaced by transitional milk. Transitional milk is a creamy liquid that lasts for approximately two weeks and includes high levels of fat, lactose, and water-soluble vitamins. It also contains more calories than colostrum. After a new mother begins to produce transitional milk, she typically notices a change in the volume and type of liquid secreted and an increase in the weight and size of her breasts.American Pregnancy Association. “Breastfeeding: Overview.” Last updated January 2012. http://www.americanpregnancy.org/firstyearoflife/breastfeedingoverview.htm.
Mature Milk
Mature milk is the final fluid that a new mother produces. In most women, it begins to secrete at the end of the second week postchildbirth. There are two types of mature milk that appear during a feeding. Foremilk occurs at the beginning and includes water, vitamins, and protein. Hind-milk occurs after the initial release of milk and contains higher levels of fat, which is necessary for weight gain. Combined, these two types of milk ensure that a baby receives adequate nutrients to grow and develop properly.American Pregnancy Association. “Breastfeeding: Overview.” Last updated January 2012. http://www.americanpregnancy.org/firstyearoflife/breastfeedingoverview.htm.
About 90 percent of mature milk is water, which helps an infant remain hydrated. The other 10 percent contains carbohydrates, proteins, and fats, which support energy and growth. Similar to cow’s milk, the main carbohydrate of mature breast milk is lactose. Breast milk contains vital fatty acids, such as docosahexaenoic acid (DHA) and arachidonic acid (ARA). In terms of protein, breast milk contains more whey than casein (which is the reverse of cow’s milk). Whey is much easier for infants to digest than casein. Complete protein, which means all of the essential amino acids, is also present in breast milk. Complete protein includes lactoferrin, an iron-gathering compound that helps to absorb iron into an infant’s bloodstream.
In addition, breast milk provides adequate vitamins and minerals. Although absolute amounts of some micronutrients are low, they are more efficiently absorbed by infants. Other essential components include digestive enzymes that help a baby digest the breast milk. Human milk also provides the hormones and growth factors that help a newborn to develop.
Diet and Milk Quality
A mother’s diet can have a major impact on milk production and quality. As during pregnancy, lactating mothers should avoid illegal substances and cigarettes. Some legal drugs and herbal products can be harmful as well, so it is helpful to discuss them with a health-care provider. Some mothers may need to avoid certain things, such as spicy foods, that can produce gas in sensitive infants. Lactating women can drink alcohol, though they must avoid breastfeeding until the alcohol has completely cleared from their milk. Typically, this takes two to three hours for 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of liquor, depending on a woman’s body weight.Harms, R., MD. “Breast-Feeding and Alcohol: Is It Okay to Drink?” © 1998–2012 Mayo Foundation for Medical Education and Research. Accessed February 21, 2012. http://www.mayoclinic.com/health/breast-feeding-and-alcohol/AN02131. Precautions are necessary because exposure to alcohol can disrupt an infant’s sleep schedule.
Benefits of Breastfeeding
Breastfeeding has a number of benefits, both for the mother and for the child. Breast milk contains immunoglobulins, enzymes, immune factors, and white blood cells. As a result, breastfeeding boosts the baby’s immune system and lowers the incidence of diarrhea, along with respiratory diseases, gastrointestinal problems, and ear infections. Breastfed babies also are less likely to develop asthma and allergies, and breastfeeding lowers the risk of sudden infant death syndrome. In addition, human milk encourages the growth of healthy bacteria in an infant’s intestinal tract. All of these benefits remain in place after an infant has been weaned from breast milk. Some studies suggest other possible long-term effects. For example, breast milk may improve an infant’s intelligence and protect against Type 1 diabetes and obesity, although research is ongoing in these areas.Healthy Children.org. “Breastfeeding Benefits Your Baby’s Immune System.” © 2012 American Academy of Pediatrics. Accessed February 21, 2012. http://www.healthychildren.org/English/ages-stages/baby/breastfeeding/pages/Breastfeeding-Benefits-Your-Baby%27s-Immune-System.aspx.
Breastfeeding has a number of other important benefits. It is easier for babies to digest breast milk than bottle formula, which contains proteins made from cow’s milk that require an adjustment period for infant digestive systems. Breastfed infants are sick less often than bottle-fed infants. Breastfeeding is more sustainable and results in less plastic waste and other trash. Breastfeeding can also save families money because it does not incur the same cost as purchasing formula. Other benefits include that breast milk is always ready. It does not have to be mixed, heated, or prepared. Also, breast milk is sterile and is always at the right temperature.
In addition, the skin-to-skin contact of breastfeeding promotes a close bond between mother and baby, which is an important emotional and psychological benefit. The practice also provides health benefits for the mother. Breastfeeding helps a woman’s bones stay strong, which protects against fractures later in life. Studies have also shown that breastfeeding reduces the risk of breast and ovarian cancers.National Cancer Institute. “Reproductive History and Breast Cancer Risk.” Accessed February 6, 2012. http://www.cancer.gov/cancertopics/factsheet/Risk/reproductive-history.
The Baby-Friendly Hospital Initiative
In 1991, the WHO and UNICEF launched the Baby-Friendly Hospital Initiative (BFHI), which works to ensure that all maternities, including hospitals and free-standing facilities, become centers of breastfeeding support. A maternity can be denoted as “baby-friendly” when it does not accept substitutes to human breast milk and has implemented ten steps to support breastfeeding. These steps include having a written policy on breastfeeding communicated to health-care staff on a routine basis, informing all new mothers about the benefits and management of breastfeeding, showing new mothers how to breastfeed their infants, and how to maintain lactation, and giving newborns no food or drink other than breast milk, unless medically indicated. Since the BFHI began, more than fifteen thousand facilities in 134 countries, from Benin to Bangladesh, have been deemed “baby friendly.” As a result, more mothers are breastfeeding their newborns and infant health has improved, in both the developed world and in developing nations.United Nations Children’s Fund. “The Baby-Friendly Hospital Initiative.” Accessed June 8, 2012. http://www.unicef.org/programme/breastfeeding/baby.htm.
Barriers to Breastfeeding
Although breast milk is ideal for almost all infants, there are some challenges that nursing mothers may face when starting and continuing to breastfeed their infants. These obstacles include painful engorgement or fullness in the breasts, sore and tender nipples, lack of comfort or confidence in public, and lack of accommodation to breastfeed or express milk in the workplace.
One of the first challenges nursing mothers face is learning the correct technique. It may take a little time for a new mother to help her baby properly latch on to her nipples. Improper latching can result in inadequate intake, which could slow growth and development. However, International Board Certified Lactation Consultants (IBCLCs), OB nurses, and registered dietitians are all trained to help new mothers learn the proper technique. Education, the length of maternity leave, and laws to protect public breastfeeding, among other measures, can all help to facilitate breastfeeding for many lactating women and their newborns.
Contraindications to Breastfeeding
Although there are numerous benefits to breastfeeding, in some cases there are also risks that must be considered. In the developed world, a new mother with HIV should not breastfeed, because the infection can be transmitted through breast milk. These women typically have access to bottle formula that is safe, and can be used as a replacement for breast milk. However, in developing nations where HIV infection rates are high and acceptable infant formula can be difficult to come by, many newborns would be deprived of the nutrients they need to develop and grow. Also, inappropriate or contaminated bottle formulas cause 1.5 million infant deaths each year. As a result, the WHO recommends that women infected with HIV in the developing world should nurse their infants while taking antiretroviral medications to lower the risk of transmission.World Health Organization. “Infant and Young Child Feeding.” July 2010. http://www.who.int/mediacentre/factsheets/fs342/en/index.html
Breastfeeding also is not recommended for women undergoing radiation or chemotherapy treatment for cancer. Additionally, if an infant is diagnosed with galactosemia, meaning an inability to process the simple sugar galactose, the child must be on a galactose-free diet, which excludes breast milk. This genetic disorder is a very rare condition, however, and only affects 1 in thirty- to sixty thousand newborns.Genetics Home Reference, a service of the US National Library of Medicine. “Galactosemia.” July 9, 2012. http://ghr.nlm.nih.gov/condition/galactosemia. When breastfeeding is contraindicated for any reason, feeding a baby formula enables parents and caregivers to meet their newborn’s nutritional needs.
Bottle-Feeding
Most women can and should breastfeed when given sufficient education and support. However, as discussed, a small percentage of women are unable to breastfeed their infants, while others choose not to. For parents who choose to bottle-feed, infant formula provides a balance of nutrients. However, not all formulas are the same and there are important considerations that parents and caregivers must weigh. Standard formulas use cow’s milk as a base. They have 20 calories per fluid ounce, similar to breast milk, with vitamins and minerals added. Soy-based formulas are usually given to infants who develop diarrhea, constipation, vomiting, colic, or abdominal pain, or to infants with a cow’s milk protein allergy. Hypoallergenic protein hydrolysate formulas are usually given to infants who are allergic to cow’s milk and soy protein. This type of formula uses hydrolyzed protein, meaning that the protein is broken down into amino acids and small peptides, which makes it easier to digest. Preterm infant formulas are given to low birth weight infants, if breast milk is unavailable. Preterm infant formulas have 24 calories per fluid ounce and are given until the infant reaches a desired weight.
Infant formula comes in three basic types:
- Powder that requires mixing with water. This is the least expensive type of formula.
- Concentrates, which are liquids that must be diluted with water. This type is slightly more expensive.
- Ready-to-use liquids that can be poured directly into bottles. This is the most expensive type of formula. However, it requires the least amount of preparation. Ready-to-use formulas are also convenient for traveling.
Most babies need about 2.5 ounces of formula per pound of body weight each day. Therefore, the average infant should consume about 24 fluid ounces of breast milk or formula per day. When preparing formula, parents and caregivers should carefully follow the safety guidelines, since an infant has an immature immune system. All equipment used in formula preparation should be sterilized. Prepared, unused formula should be refrigerated to prevent bacterial growth. Parents should make sure not to use contaminated water to mix formula in order to prevent foodborne illnesses. Follow the instructions for powdered and concentrated formula carefully—formula that is overdiluted would not provide adequate calories and protein, while overconcentrated formula provides too much protein and too little water which can impair kidney function.
It is important to note again that both the American Academy of Pediatrics and the WHO state that breast milk is far superior to infant formula. This table compares the advantages of giving a child breast milk to the disadvantages of using bottle formula.
Table 12.4 Breast Milk versus Bottle Formula
| Breast Milk | Bottle Formula |
|---|---|
| Antibodies and lactoferrin in breast milk protect infants. | Formula does not contain immunoprotective factors. |
| The iron in breast milk is absorbed more easily. | Formula contains more iron than breast milk, but it is not absorbed as easily. |
| The feces that babies produce do not smell because breastfed infants have different bacteria in the gut. | The feces that bottle-fed infants produce tends to have a foul-smelling odor. |
| Breast milk is always available and is always at the correct temperature. | Formula must be prepared, refrigerated for storage, and warmed before it is given to an infant. |
| Breastfed infants are less likely to have constipation. | Bottle-fed infants are more likely to have constipation. |
| Breastfeeding ostensibly is free, though purchasing a pump and bottles to express milk does require some expense. | Formula must be purchased and is expensive. |
| Breast milk contains the fatty acids DHA and ARA, which are vital for brain and vision development. | Some formulas contain DHA and ALA. |
Source: American Pregnancy Association. “Breastfeeding versus Bottle Feeding.” November 5, 2012. http://www.americanpregnancy.org/firstyearoflife/breastfeedingandbottle.html.
Video 12.3
Breastfeeding Mothers—La Leche League Canada
(click to see video)This video explains the benefits of breastfeeding for both mothers and infants.
Introducing Solid Foods
Infants should be breastfed or bottle-fed exclusively for the first six months of life according to the WHO. (The American Academy of Pediatrics recommends breast milk or bottle formula exclusively for at least the first four months, but ideally for six months.) Infants should not consume solid foods prior to six months because solids do not contain the right nutrient mix that infants need. Also, eating solids may mean drinking less breast milk or bottle formula. If that occurs, an infant may not consume the right quantities of various nutrients. If parents try to feed an infant who is too young or is not ready, their tongue will push the food out, which is called an extrusion reflexAn involuntary reflex that causes infants to push food out of their mouths with their tongues.. After six months, the suck-swallow reflexes are not as strong, and infants can hold up their heads and move them around, both of which make eating solid foods more feasible.
Solid baby foods can be bought commercially or prepared from regular food using a food processor, blender, food mill, or grinder at home. Usually, an infant cereal can be offered from a spoon between four to six months. By nine months to a year, infants are able to chew soft foods and can eat solids that are well chopped or mashed.
Infants who are fed solid foods too soon are susceptible to developing food allergies. Therefore, as parents and caregivers introduce solids, they should feed their child only one new food at a time (starting with rice cereal, followed by fruits or vegetables), to help identify allergic responses or food intolerances. An iron supplement or iron-fortified cereal is also recommended at this time.
Learning to Self-Feed
With the introduction of solid foods, young children begin to learn how to handle food and how to feed themselves. At six to seven months, infants can use their whole hand to pick up items (this is known as the palmer graspA grip that involves picking up an object with the whole hand.). They can lift larger items, but picking up smaller pieces of food is difficult. At eight months, a child might be able to use a pincer graspA grip that involves picking up an object with the fingers., which uses fingers to pick up objects. After the age of one, children slowly begin to use utensils to handle their food. Unbreakable dishes and cups are essential, since very young children may play with them or throw them when they become bored with their food.
Feeding Problems during Infancy
Parents and caregivers should be mindful of certain diet-related problems that may arise during infancy. Certain foods are choking hazards, including foods with skins or foods that are very small, such as grapes. Other examples of potential choking hazards include raw carrots and apples, raisins, and hard candy. Parents should also avoid adding salt or seasonings to an infant’s food.
Heating an infant’s food presents a risk of accidental injury or burns, which may occur if the food is heated unevenly or excessively. Keep in mind that an infant cannot communicate that the food is too hot. Also, parents and caregivers should never leave a baby alone at mealtime, because an infant can accidentally choke on pieces of food that are too big or have not been adequately chewed. Raw honey and corn syrup both contain spores of Clostridium botulinum. They produce a poisonous toxin in a baby’s intestines, which can cause the foodborne illness botulism. After the age of one, it is safe to give an infant honey or corn syrup. However, honey as an ingredient in food, such as in cereal, is safe for all ages because it has been adequately heat treated.
Overnutrition
Overnutrition during infancy is a growing problem. Overfed infants may develop dietary habits and metabolic characteristics that last a lifetime. According to the American Journal of Clinical Nutrition, the consequences of overnutrition and growth acceleration in infancy include long-term obesity, along with Type 2 diabetes and cardiovascular disease later in life.Singhal, A. et al. “Nutrition in Infancy and Long-Term Risk of Obesity: Evidence from Two Randomized Control Trials.” Am J Clin Nutr 92 (2010): 1133–44. Therefore, parents and other caregivers should restrain from overfeeding, and ideally give their infants breast milk to promote health and well-being.
Food Allergies
Food allergies impact four to six percent of young children in America. Common food allergens that can appear just before or after the first year include peanut butter, egg whites, wheat, cow’s milk, and nuts. For infants, even a small amount of a dangerous food can prove to be life-threatening. If there is a family history of food allergies, it is a good idea to delay giving a child dairy products until one year of age, eggs until two years of age, and shellfish, fish, and nuts until three years of age.
However, lactating women should not make any changes to their diets. Research shows that nursing mothers who attempt to ward off allergies in their infants by eliminating certain foods may do more harm than good. According to the American Academy of Allergy, Asthma, and Immunology, mothers who avoided certain dairy products showed decreased levels in their breast milk of an immunoglobulin specific to cow’s milk. This antibody is thought to protect against the development of allergies in children. Even when an infant is at higher risk for food allergies, there is no evidence that alterations in a mother’s diet make a difference.Gever, J. “Nursing Mom’s Diet No Guard Against Baby Allergies.” Medpage Today. © 2012 Everyday Health, Inc. March 7, 2012. http://www.medpagetoday.com/MeetingCoverage/AAAAIMeeting/31527?utm_content=&utm_medium=email&utm _campaign=DailyHeadlines&utm_source=WC&eun=g330425d0r&userid=330425& email=mzimmerman@cox.net&mu_id=.
Early Childhood Caries
Primary teeth are at risk for a disorder known as early childhood cariesA dental disorder characterized by decay within the primary teeth. from breast milk, formula, juice, or other drinks fed through a bottle. Liquids can build up in a baby’s mouth, and the natural or added sugars lead to decay. Early childhood caries is caused not only by the kinds of liquids given to an infant, but also by the frequency and length of time that fluids are given. Giving a child a bottle of juice or other sweet liquids several times each day, or letting a baby suck on a bottle longer than a mealtime, either when awake or asleep, can also cause early childhood caries. In addition, this practice affects the development and position of the teeth and the jaw. The risk of early childhood caries continues into the toddler years as children begin to consume more foods with a high sugar content. Therefore, parents should avoid giving their children sugary snacks and beverages.
Gastroesophageal Reflux
Small amounts of spitting up during a feeding is normal. However, there is cause for concern if it is too difficult to feed an infant due to gastroesophageal refluxA disorder that occurs when stomach acid rises into the esophagus. In infancy, it is characterized by coughing, choking, or vomiting after feeding.. This condition occurs when stomach muscles open at the wrong times and allow milk or food to back up into the esophagus. Symptoms of gastroesophagel reflux in infants include severe spitting up, projectile vomiting, arching of the back as though in pain, refusal to eat or pulling away from the breast during feedings, gagging or problems with swallowing, and slow weight gain. For most infants, making adjustments in feeding practices addresses the issue. For example, a parent can feed their baby in an upright position, wait at least an hour after eating for play time, burp more often, or give a child smaller, more frequent feedings.
Diarrhea and Constipation
Diarrhea is often caused by a gastrointestinal infection and can dehydrate an infant. It is characterized by stool frequency and consistency that deviates substantially from the norm. If an infant has had several bouts of this condition, they will need to replace lost fluids and electrolytes. A common recommendation is to give a child an oral rehydration solution. Because of the immunoprotective factors in breast milk, breastfed infants are less likely to contract gastrointestinal viral illness and experience diarrhea.
Infant constipation—which is the passage of hard, dry bowel movements, but not necessarily the absence of daily bowel movements—is another common problem. This condition frequently begins when a baby transitions from breast milk to formula or begins eating solid foods. Pediatricians can provide the best guidance for handling the problem. Common recommendations include applying a small amount of water-based lubricant to an infant’s anus to ease the passage of hard stools, and feeding an infant on solid foods pureed pears or prunes, or providing barley cereal in place of rice cereal.Mayo Clinic. “Infant and Toddler Health.” March 16, 2011. © 1998–2012 Mayo Foundation for Medical Education and Research. http://www.mayoclinic.com/health/infant-and-toddler-health/MY00362. Parents can also offer their child a little more water in between feedings to help alleviate the condition.
Colic
Colic is a common problem during infancy, characterized by crankiness and crying jags. It is defined as crying that lasts longer than three hours per day for at least three days per week and for at least three weeks (which is commonly known as the “rule of 3’s”), and is not caused by a medical problem. About one-fifth of all infants develop colic, usually between the second and third weeks. Crying spells can occur around the clock, but often worsen in the early evening. Also, colicky babies may have stomachs that are enlarged or distended with gas.
There is no definitive explanation for colic. Often, colic occurs when a child is unusually sensitive to stimulation. In breastfeeding babies, colic can be a sign of sensitivity to the mother’s diet. Lactating mothers can try to eliminate caffeine, chocolate, and any other potentially irritating foods from their meals.Medline Plus, a service of the US National Library of Medicine. “Colic and Crying.” Last updated August 2, 2011. http://www.nlm.nih.gov/medlineplus/ency/article/000978.htm. However, since colic usually subsides over time, any improvement that occurs with food elimination may conincide with the natural healing process.
Parents and caregivers who are feeding bottle formula to colicky babies should talk with pediatricians about replacing it with a protein hydrolysate formula.American Academy of Pediatrics. “Colic.” HealthyChildren.org. © American Academy of Pediatrics. Last updated May 12, 2011. http://www.healthychildren.org/English/ages-stages/baby/crying-colic/pages/Colic.aspx. Whether breastfeeding or bottle-feeding, it is also important not to overfeed infants, which could make them uncomfortable and more likely to have crying fits. In general, it is best to wait between two and three hours from the start of one feeding to the start of the next. If food sensitivity is the cause, colic should cease within a few days of making changes. Eventually, the problem goes away. Symptoms usually begin to dissipate after six weeks and are gone by twelve weeks.Medline Plus, a service of the US National Library of Medicine. “Colic and Crying.” Last updated August 2, 2011. http://www.nlm.nih.gov/medlineplus/ency/article/000978.htm.
Newborn Jaundice

Yellowing skin is one sign of newborn jaundice.
© Thinkstock
Newborn jaundiceA condition that can occur within a few days of birth and is characterized by yellowed skin or yellowing in the whites of the eyes. is another potential problem during infancy. This condition can occur within a few days of birth and is characterized by yellowed skin or yellowing in the whites of the eyes, which can be harder to detect in dark-skinned babies. Jaundice typically appears on the face first, followed by the chest, abdomen, arms, and legs. This disorder is caused by elevated levels of bilirubin in a baby’s bloodstream. Bilirubin is a substance created by the breakdown of red blood cells and is removed by the liver. Jaundice develops when a newborn’s liver does not efficiently remove bilirubin from the blood. There are several types of jaundice associated with newborns:
- Physiologic jaundice. The most common type of newborn jaundice and can affect up to 60 percent of full-term babies in the first week of life.
- Breast-milk jaundice. The name for a condition that persists after physiologic jaundice subsides in otherwise healthy babies and can last for three to twelve weeks after birth. Breast-milk jaundice tends to be genetic and there is no known cause, although it may be linked to a substance in the breast milk that blocks the breakdown of bilirubin. However, that does not mean breastfeeding should be stopped. As long as bilirubin levels are monitored, the disorder rarely leads to serious complications.
- Breastfeeding jaundice. Occurs when an infant does not get enough milk. This may happen because a newborn does not get a good start breastfeeding, does not latch on to the mother’s breast properly, or is given other substances that interfere with breastfeeding (such as juice). Treatment includes increased feedings, with help from a lactation consultant to ensure that the baby takes in adequate amounts.
Newborn jaundice is more common in a breastfed baby and tends to last a bit longer. If jaundice is suspected, a pediatrician will run blood tests to measure the amount of bilirubin in an infant’s blood. Treatment often involves increasing the number of feedings to increase bowel movements, which helps to excrete bilirubin. Within a few weeks, as the baby begins to mature and red blood cell levels diminish, jaundice typically subsides with no lingering effects.American Pregnancy Association. “Breastfeeding and Jaundice.” © 2000–2012 American Pregnancy Association. Accessed February 21, 2012. http://www.americanpregnancy.org/firstyearoflife/breastfeedingandjaundice.htm.
Key Takeaways
- Parents and other caregivers should use growth charts to track an infant’s development and determine how to best meet their child’s nutritional needs.
- For the first four to six months of life, children should consume breast milk exclusively. For the next six months, solid foods should be introduced gradually into an infant’s diet as parents and caregivers continue to provide breast milk.
- Breast milk is ideal for infants and provides all of the nutrients they need to grow and develop.
- Breastfeeding provides a number of benefits for both a mother and her infant. For babies, breast milk boosts the immune system to protect against disease. For mothers, breastfeeding has several health benefits, such as reducing the risk of breast cancer and ovarian cancer. For both, breastfeeding promotes an emotional bond between mother and child.
- Some problems related to food and nutrition that may occur during infancy include overnutrition, early childhood caries, gastroesophageal reflux, diarrhea, constipation, and colic.
Discussion Starter
- Why do some women choose to breastfeed their infants? Why do others decline to breastfeed? Discuss this crucial decision that parents make in the first stages of an infant’s life and the possible consequences of each choice.
12.4 Nutrition in the Toddler Years
Learning Objectives
- Summarize nutritional requirements and dietary recommendations for toddlers.
- Explore the introduction of solid foods into a toddler’s diet.
- Examine feeding problems that parents and caregivers may face with their toddlers.
By the age of two, children have advanced from infancy and are on their way to becoming school-aged children. Their physical growth and motor development slows compared to the progress they made as infants. However, toddlers experience enormous intellectual, emotional, and social changes. Of course, food and nutrition continue to play an important role in a child’s development. During this stage, the diet completely shifts from breastfeeding or bottle-feeding to solid foods along with healthy juices and other liquids. Parents of toddlers also need to be mindful of certain nutrition-related issues that may crop up during this stage of the human life cycle. For example, fluid requirements relative to body size are higher in toddlers than in adults because children are at greater risk of dehydration. Toddlers should drink about 1.3 liters of fluids per day, ideally liquids that are low in sugar.
The Toddler Years (Ages Two to Three)
During this phase of human development, children are mobile and grow more slowly than infants, but are much more active. The toddler years pose interesting challenges for parents or other caregivers, as children learn how to eat on their own and begin to develop personal preferences. However, with the proper diet and guidance, toddlers can continue to grow and develop at a healthy rate.
Nutritional Requirements
MyPlate may be used as a guide for the toddler’s diet (http://www.choosemyplate.gov/preschoolers.html). A toddler’s serving sizes should be approximately one-quarter that of an adult’s. One way to estimate serving sizes for young children is one tablespoon for each year of life. For example, a two-year-old child would be served 2 tablespoons of fruits or vegetables at a meal, while a four-year-old would be given 4 tablespoons, or a quarter cup. Here is an example of a toddler-sized meal:
- 1 ounce of meat or chicken, or 2 to 3 tablespoons of beans
- One-quarter slice of whole-grain bread
- 1 to 2 tablespoons of cooked vegetable
- 1 to 2 tablespoons of fruit
Energy
The energy requirements for ages two to three are about 1,000 to 1,400 calories a day. In general, a toddler needs to consume about 40 calories for every inch of height. For example, a young child who measures 32 inches should take in an average of 1,300 calories a day. However, the recommended caloric intake varies with each child’s level of activity. Toddlers require small, frequent, nutritious snacks and meals to satisfy energy requirements. The amount of food a toddler needs from each food group depends on daily calorie needs. See Table 12.5 "Serving Sizes for Toddlers" for some examples.
Table 12.5 Serving Sizes for Toddlers
| Food Group | Daily Serving | Examples |
|---|---|---|
Grains |
About 3 ounces of grains per day, ideally whole grains |
|
Proteins |
2 ounces of meat, poultry, fish, eggs, or legumes |
|
Fruits |
1 cup of fresh, frozen, canned, and/or dried fruits, or 100 percent fruit juice |
|
Vegetables |
1 cup of raw and/or cooked vegetables |
|
Dairy Products |
2 cups per day |
|
Source: Academy of Nutrition and Dietetics. “It‘s about Eating Right: Size-Wise Nutrition for Toddlers.” © 1995–2012, Academy of Nutrition and Dietetics, all rights reserved. http://www.eatright.org/public/content.aspx?id=8055.
Macronutrients
For carbohydrate intake, the Acceptable Macronutrient Distribution Range (AMDR) is 45 to 65 percent of daily calories (113 to 163 grams for 1,000 daily calories). Toddlers’ needs increase to support their body and brain development. Brightly-colored unrefined carbohydrates, such as peas, orange slices, tomatoes, and bananas are not only nutrient-dense, they also make a plate look more appetizing and appealing to a young child. The RDA of protein is 5 to 20 percent of daily calories (13 to 50 grams for 1,000 daily calories). The AMDR for fat for toddlers is 30 to 40 percent of daily calories (33 to 44 grams for 1,000 daily calories). Essential fatty acids are vital for the development of the eyes, along with nerve and other types of tissue. However, toddlers should not consume foods with high amounts of trans fats and saturated fats. Instead, young children require the equivalent of 3 teaspoons of healthy oils, such as canola oil, each day.
Micronutrients
As a child grows bigger, the demands for micronutrients increase. These needs for vitamins and minerals can be met with a balanced diet, with a few exceptions. According to the American Academy of Pediatrics, toddlers and children of all ages need 600 international units of vitamin D per day. Vitamin D-fortified milk and cereals can help to meet this need. However, toddlers who do not get enough of this micronutrient should receive a supplement. Pediatricians may also prescribe a fluoride supplement for toddlers who live in areas with fluoride-poor water. Iron deficiency is also a major concern for children between the ages of two and three. You will learn about iron-deficiency anemia later in this section.
Learning How to Handle Food

As toddlers mature, they become more comfortable handling dishes and utensils.
© Thinkstock
As children grow older, they enjoy taking care of themselves, which includes self-feeding. During this phase, it is important to offer children foods that they can handle on their own and that help them avoid choking and other hazards. Examples include fresh fruits that have been sliced into pieces, orange or grapefruit sections, peas or potatoes that have been mashed for safety, a cup of yogurt, and whole-grain bread or bagels cut into pieces. Even with careful preparation and training, the learning process can be messy. As a result, parents and other caregivers can help children learn how to feed themselves by providing the following:
- small utensils that fit a young child’s hand
- small cups that will not tip over easily
- plates with edges to prevent food from falling off
- small servings on a plate
- high chairs, booster seats, or cushions to reach a table
Feeding Problems in the Toddler Years
During the toddler years, parents may face a number of problems related to food and nutrition. Possible obstacles include difficulty helping a young child overcome a fear of new foods, or fights over messy habits at the dinner table. Even in the face of problems and confrontations, parents and other caregivers must make sure their preschooler has nutritious choices at every meal. For example, even if a child stubbornly resists eating vegetables, parents should continue to provide them. Before long, the child may change their mind, and develop a taste for foods once abhorred. It is important to remember this is the time to establish or reinforce healthy habits.
Nutritionist Ellyn Satter states that feeding is a responsibility that is split between parent and child. According to Satter, parents are responsible for what their infants eat, while infants are responsible for how much they eat. In the toddler years and beyond, parents are responsible for what children eat, when they eat, and where they eat, while children are responsible for how much food they eat and whether they eat. Satter states that the role of a parent or a caregiver in feeding includes the following:
- selecting and preparing food
- providing regular meals and snacks
- making mealtimes pleasant
- showing children what they must learn about mealtime behavior
- avoiding letting children eat in between meal- or snack-timesEllyn Satter Associates. “Ellyn Satter’s Division of Responsibility in Feeding.” © 2012 by Ellyn Satter. http://www.ellynsatter.com/ellyn-satters-division-of-responsibility -in-feeding-i-80.html.
High-Risk Choking Foods
Certain foods are difficult for toddlers to manage and pose a high risk of choking. Big chunks of food should not be given to children under the age of four. Also, globs of peanut butter can stick to a younger child’s palate and choke them. Popcorn and nuts should be avoided as well, because toddlers are not able to grind food and reduce it to a consistency that is safe for swallowing. Certain raw vegetables, such as baby carrots, whole cherry tomatoes, whole green beans, and celery are also serious choking hazards. However, there is no reason that a toddler cannot enjoy well-cooked vegetables cut into bite-size pieces.
Picky Eaters
The parents of toddlers are likely to notice a sharp drop in their child’s appetite. Children at this stage are often picky about what they want to eat. They may turn their heads away after eating just a few bites. Or, they may resist coming to the table at mealtimes. They also can be unpredictable about what they want to consume for specific meals or at particular times of the day. Although it may seem as if toddlers should increase their food intake to match their level of activity, there is a good reason for picky eating. A child’s growth rate slows after infancy, and toddlers ages two and three do not require as much food.
Food Jags
For weeks, toddlers may go on a food jagA behavior exhibited by a young child who insists upon eating the same foods over and over again. and eat one or two preferred foods—and nothing else. It is important to understand that preferences will be inconsistent as a toddler develops eating habits. This is one way that young children can assert their individuality and independence. However, parents and caregivers should be concerned if the same food jag persists for several months, instead of several weeks. Options for addressing this problem include rotating acceptable foods while continuing to offer diverse foods, remaining low-key to avoid exacerbating the problem, and discussing the issue with a pediatrician. Also, children should not be forced to eat foods that they do not want. It is important to remember that food jags do not have a long-term effect on a toddler’s health, and are usually temporary situations that will resolve themselves.
Toddler Obesity
Another potential problem during the early childhood years is toddler obesity. According to the US Department of Health and Human Services, in the past thirty years, obesity rates have more than doubled for all children, including infants and toddlers.Head Start, US Department of Health and Human Services. “Prevention of Overweight and Obesity in Infants and Toddlers.” 2005. Accessed February 21, 2012. http://eclkc.ohs.acf.hhs.gov/hslc/tta-system/family Almost 10 percent of infants and toddlers weigh more than they should considering their length, and slightly more than 20 percent of children ages two to five are overweight or obese.Institute of Medicine of the National Academies. “Early Childhood Obesity Prevention Policies.” June 23, 2011. http://www.iom.edu/Reports/2011/Early-Childhood -Obesity-Prevention-Policies.aspx Obesity during early childhood tends to linger as a child matures and cause health problems later in life.
There are a number of reasons for this growing problem. One is a lack of time. Parents and other caregivers who are constantly on the go may find it difficult to fit home-cooked meals into a busy schedule and may turn to fast food and other conveniences that are quick and easy, but not nutritionally sound. Another contributing factor is a lack of access to fresh fruits and vegetables. This is a problem particularly in low-income neighborhoods where local stores and markets may not stock fresh produce or may have limited options. Physical inactivity is also a factor, as toddlers who live a sedentary lifestyle are more likely to be overweight or obese. Another contributor is a lack of breastfeeding support. Children who were breastfed as infants show lower rates of obesity than children who were bottle-fed.
To prevent or address toddler obesity parents and caregivers can do the following:
- Eat at the kitchen table instead of in front of a television to monitor what and how much a child eats.
- Offer a child healthy portions. The size of a toddler’s fist is an appropriate serving size.
- Plan time for physical activity, about sixty minutes or more per day. Toddlers should have no more than sixty minutes of sedentary activity, such as watching television, per day.
Early Childhood Caries
Early childhood caries remains a potential problem during the toddler years. The risk of early childhood caries continues as children begin to consume more foods with a high sugar content. According to the National Health and Nutrition Examinaton Survey, children between ages of two and five consume about 200 calories of added sugar per day.US Department of Health and Human Services. “Consumption of Added Sugar among US Children and Adolescents.” NCHS Data Brief, No. 87 (March 2012). Therefore, parents with toddlers should avoid processed foods, such as snacks from vending machines, and sugary beverages, such as soda. Parents also need to instruct a child on brushing their teeth at this time to help a toddler develop healthy habits and avoid tooth decay.
Iron-Deficiency Anemia
An infant who switches to solid foods, but does not eat enough iron-rich foods, can develop iron-deficiency anemiaA condition characterized by inadequate hemoglobin in the blood due to low iron levels.. This condition occurs when an iron-deprived body cannot produce enough hemoglobin, a protein in red blood cells that transports oxygen throughout the body. The inadequate supply of hemoglobin for new blood cells results in anemia. Iron-deficiency anemia causes a number of problems including weakness, pale skin, shortness of breath, and irritability. It can also result in intellectual, behavioral, or motor problems. In infants and toddlers, iron-deficiency anemia can occur as young children are weaned from iron-rich foods, such as breast milk and iron-fortified formula. They begin to eat solid foods that may not provide enough of this nutrient. As a result, their iron stores become diminished at a time when this nutrient is critical for brain growth and development.
There are steps that parents and caregivers can take to prevent iron-deficiency anemia, such as adding more iron-rich foods to a child’s diet, including lean meats, fish, poultry, eggs, legumes, and iron-enriched whole-grain breads and cereals. A toddler’s diet should provide 7 to 10 milligrams of iron daily. Although milk is critical for the bone-building calcium that it provides, intake should not exceed the RDA to avoid displacing foods rich with iron. Children may also be given a daily supplement, using infant vitamin drops with iron or ferrous sulfate drops. If iron-deficiency anemia does occur, treatment includes a dosage of 3 milligrams per kilogram once daily before breakfast, usually in the form of a ferrous sulfate syrup. Consuming vitamin C, such as orange juice, can also help to improve iron absorption.Kazal Jr., L. A., MD. “Prevention of Iron Deficiency in Infants and Toddlers.” American Academy of Family Physicians 66, no. 7 (October 1, 2002): 1217—25. http://www.aafp.org/afp/2002/1001/p1217.html.
Toddler Diarrhea
As with adults, a variety of conditions or circumstances may give a toddler diarrhea. Possible causes include bacterial or viral infections, food allergies, or lactose intolerance, among other medical conditions. Excessive fruit juice consumption (more than one 6-ounce cup per day) can also lead to diarrhea.American Academy of Pediatrics, Committee on Nutrition 1999–2000. “The Use and Misuse of Fruit Juice in Pediatrics.” Pediatrics 119, no. 2 (February 2007): 405. doi:10.1542/peds.2006-3222. Diarrhea presents a special concern in young children because their small size makes them more vulnerable to dehydration. Parents should contact a pediatrician if a toddler has had diarrhea for more than twenty-four hours, if a child is also vomiting, or if they exhibit signs of dehydration, such as a dry mouth or tongue, or sunken eyes, cheeks, or abdomen. Preventing or treating dehydration in toddlers includes the replacement of lost fluids and electrolytes (sodium and potassium). Oral rehydration therapy, or giving special fluids by mouth, is the most effective measure.
Developing Habits
Eating habits develop early in life. They are typically formed within the first few years and it is believed that they persist for years, if not for life. So it is important for parents and other caregivers to help children establish healthy habits and avoid problematic ones. Children begin expressing their preferences at an early age. Parents must find a balance between providing a child with an opportunity for self-expression, helping a child develop healthy habits, and making sure that a child meets all of their nutritional needs. Following Ellyn Satter’s division of responsibility in feeding (see above) can help a child eat the right amount of food, learn mealtime behavior, and grow at a healthy and predictable rate.
Bad habits and poor nutrition have an accrual effect. The foods you consume in your younger years will impact your health as you age, from childhood into the later stages of life. As a result, good nutrition today means optimal health tomorrow. In the next chapter, you will learn about how nutritional needs change from the later childhood years, through adolescence and adulthood, and into old age. The choices that you make at every age accumulate over time and greatly impact your health into the golden years.
Video 12.4
Introducing Your Toddler to New Foods
(click to see video)This video focuses on ways to encourage toddlers to try new foods.
Key Takeaways
- By the toddler years, young children are able to self-feed and begin to develop eating habits and preferences.
- The energy requirements for ages two to three are about 1,000 to 1,400 calories per day, and in general, a toddler needs to consume about 40 calories for every inch of height.
- Growth slows during the toddler years, but children are more active at this stage and undergo a great deal of intellectual, emotional, and social development.
- Some food- and nutrition-related problems that can occur during the toddler years include choking, picky eating, food jags, early childhood caries, iron-deficiency anemia, and toddler diarrhea.
Discussion Starter
- How do the nutritional needs of a child change from infancy into the toddler years? Discuss the changing needs for energy, macronutrients, and micronutrients as young children mature.
12.5 End-of-Chapter Exercises
It’s Your Turn
- Plan a day’s worth of meals for a pregnant woman that contain the RDA of vitamin C. To help determine the vitamin C content in foods, visit the USDA National Nutrient Database: http://www.nal.usda.gov/fnic/foodcomp/search.
- Create a brochure or plan a peer-to-peer campaign that encourages pregnant women to breastfeed their newborns and includes the major benefits of this practice.
-
After watching the video, which recommends snacks for adults and older children, use these ideas and what you have learned to create a list of toddler-friendly healthy snacks for parents. Take into account potential problems for young children, such as foods that are choking hazards.
Eating Healthy Snacks
Apply It
- Create a chart that compares the energy requirements and fluid recommendations for the following phases: the second trimester of pregnancy, the third trimester of pregnancy, the first six months of lactation, and the second six months of lactation.
- Visit a store and study the labels of three different brands of infant formula. Record the nutrition facts for each brand, such as the calories, amount of carbohydrates, amount of protein, and so on.
- Research ways to adjust the behavior of picky eaters at this website: http://www.healthychildren.org. Then, create a list of four to five tips for parents of toddlers. Apply Ellyn Satter’s division of responsibility as you create your suggestions.
Expand Your Knowledge
- How might statistics regarding unplanned pregnancies relate to the recommendation that all women should regularly take a multivitamin with folic acid? Use your knowledge of the impact of folate to explain your response.
- Write a short speech that you would give to local government officials to recommend ways that they can promote and support the practice of breastfeeding in your community. Or prepare an email or letter to explain to a friend or family member why you have made the choice to breastfeed your child or to support your partner in the practice of breastfeeding.
- Visit http://www.healthychildren.org and research ways to introduce solid foods into an infant’s diet. Then create an eating plan to help parents gradually introduce solids to their babies, beginning at the age of six months.




